The health of women plays a pivotal role in societal well-being and national development. In India, despite considerable progress, women face unique health challenges influenced by gender inequality, limited access to education, and economic disparities. These challenges are further exacerbated by societal norms and gender biases that often prioritise men’s health needs vs women’s (ICMR, 2018).
Compliance with the therapeutic regimen is crucial for controlling the viral load, reducing the risk of transmission, and improving health outcomes. Compliance also has a role in enhancing health-related quality of life (HRQoL), long-term HIV care, and management. The burden of noncommunicable diseases (NCDs) is high among women, who face ongoing health challenges due to conditions like diabetes and hypertension, cardiovascular disease, renal disease, and stroke. It is essential to adhere to treatment and consistently monitor these conditions to effectively manage NCDs and sustain a high quality of life (WHO, 2023).
Need for the study:
Compliance with treatment plans is usually linked to better health-related quality of life. The investigators observed that many women ageing with chronic conditions having not complied with the treatment regimen were readmitted to the hospital. Hence this study was undertaken.
Objectives
The study was carried out to:
(a) Assess compliance with the therapeutic regimen among women ageing with and without HIV;
(b) Assess HRQoL among women ageing with and without HIV;
(c) Correlate compliance with the therapeutic regimen and the HRQoL; and
(d) Associate compliance with the therapeutic regimen and HRQoL among women ageing with and without HIV with selected demographic and clinical variables.
Review of Literature
In a descriptive study on adherence to ART in 99 HIV/AIDS patients, Souza et al (2020) found that 52.5 percent of the patients exhibited good adherence to the therapy, and 33.3 percent had low adherence. Various factors found linked with good adherence were recognising the benefits of the treatment, experiencing minimal side effects, and having a positive self-assessment. The barrier was a lack of knowledge about the medication. Yoon et al (2023) conducted a qualitative study regarding factors influencing medication adherence using in-depth interviews with 25 patients with chronic conditions from a community hospital in Singapore. The study revealed that factors like side effects, poor understanding of medication, forgetfulness, and cultural beliefs influenced medication adherence. The study highlighted the need for a person-centred approach that includes patient education, better communication, and cultural competence training to improve medication adherence.
Girma et al (2022) conducted a cross-sectional study on the HRQoL of 426 HIV positive women receiving ART in public hospitals in central Ethiopia. This study found that HIV-positive women on ART had poor HRQoL, with factors such as depression, post-traumatic stress disorder, older age, rural residence, and bedridden status negatively impacting HRQoL. Conversely, good treatment adherence was positively associated with better HRQoL. Al-Noumani et al (2022) conducted a national cross-sectional study on factors affecting the HRQoL in patients with NCDs. The study included 800 participants diagnosed with six different NCDs. The findings revealed that higher medication adherence was linked to improved physical and role functioning as well as better mental health. Social support and good health literacy were also found to positively impact various aspects of HRQoL.
Opara HC (2022) revealed in a crosssectional descriptive study on the factors influencing adherence to ART among HIV-positive women attending a retroviral clinic in Enugu that the influencing factors were insufficient transportation funds, long distance to the clinic, the health worker's poor attitude, and lack of parental support. This study concluded that adherence to ART was low among women attending the HIV clinic. Cabrer DM, Chen M, et al (2022) revealed that women ageing with HIV experienced significantly lower scores in physical and mental well-being compared to their counterparts without HIV. This study highlighted the urgent need for a comprehensive approach to address the QoL issues faced by women ageing with HIV.
Materials and Methods
A quantitative research approach with a descriptive cross-sectional design was adopted as it was appropriate for comparing two distinct groups of women ageing with HIV and without HIV at a single point in time. The study was set in outpatient clinics in the Infectious Disease Medical Centre (IDMC) at VHS, Taramani, and the Madras South Lions Club Charitable Trust Hospital, Thiruvanmiyur. The study population consisted of 200 women (100 women ageing with HIV and 100 women ageing with NCDs). The sample size was calculated based on prior studies and pilot data, assuming a minimum clinically significant difference in health-related quality of life scores of 10 with a standard deviation of 20, a 5 percent level of significance, and 80 percent power.
Inclusion criteria-
Women ageing with HIV: Women diagnosed with stage I or II HIV, receiving ART for at least 6 months and on ART treatment for 6 months or above; ability to understand and speak Tamil and English; willingness to participate; attending the infectious disease OPD; women having associated medical conditions such as diabetes, hypertension, heart disease, stroke, and chronic renal disease, were included.
Exclusion criteria: Women ageing with and without HIV who were critically ill or hospitalised during the data collection period; participants of the pilot study were excluded.
Sampling technique:
A non-probability convenience sampling was used to select the samples.
Data collection and tool:
An interview was conducted using an interview schedule, and record analysis was done to collect the data. The tool prepared was based on the information gathered from the review of the literature and the objectives of the study. A 3-point rating scale consisting of 15 questions (score range: 15-45) was used to assess compliance with the therapeutic regimen. The questions covered various aspects such as medication-related factors, dietary factors, social and support system factors, access and financial factors, and psychological or emotional factors. The scale legends were Never (3), Sometimes (2), Always (1). Then, the percentage was calculated and the scores were interpreted as a good level of compliance (67-100%), Fair level of compliance (34-66%) and Poor level of compliance (≤33%). Total score was 3600. The SF-36 Survey scale consisted of 36 questions both positive (22) and negative (14) under eight categories such as physical functioning (10), body pain (2), role limitations due to personal (4) or emotional problems (3), well-being (5), social functioning (2), energy/fatigue (4), and general health (6) was used to assess the HRQoL among women aging with and without HIV. The scoring has been appropriately adjusted between 0-100 for each domain. The tool was validated by three medicalsurgical nursing experts and one medical expert. The test-retest method was used to find out the reliability of compliance with the therapeutic regimen and the HRQoL tool. The reliability scores were r = 0.95 and r=0.87 for the compliance with the therapeutic regimen and HRQoL tool, respectively. This showed that the tool was highly reliable and feasible.
The study was approved by the College ethical committee. Prior permission was obtained from the Hospital to conduct the study. Informed consent was obtained from the samples. Confidentiality and anonymity were maintained, and samples were informed of their right to withdraw from the study any time. It took approximately 35 minutes to collect the data from each sample.
Results
Demographic variables of women ageing with and without HIV: Women ageing with and without majority (48% & 43%) were between 40-45 years and 56-60 years; 39 percent of them had primary education and no formal education, 65 percent and 47 percent were homemakers among women ageing with and without HIV, respectively. The majority (81% & 74%) were Hindus, 71 percent and 66 percent were married, 55 percent and 80 percent were from urban areas, 81 percent and 60 percent belonged to a nuclear family among women aged with and without HIV, respectively. The majority (80% & 59%) had a family monthly income of more than Rs 15,000, 87 percent and 95 percent were non-vegetarian, 45 percent & 37 percent had a family history of diabetes among women ageing with and without HIV, respectively Clinical variables of women ageing with HIV: Analysis of demographic variables of women aging with HIV showed that out of 100 women, height of 63 women ranged between 151-160 cm, 60 of them weighed between 51-70 kg, 43 had a BMI between 19-25, and 69 of them were diagnosed HIV positive between 20-30 years, 88 had an undetectable viral load; 36 had a CD4 cell count between 200 and less than 500 cells/mm3, 88 of them acquired the infection through sexual transmission, 76 had the disease for more than 10 years, 70 were on ART for more than 10 years; 44 had other illnesses like gastric ulcers, anaemia, hypothyroidism, and neuropathy, 74 had associated illnesses for less than 5 years, 78 were taking medications for less than 5 years, 74 were taking medication twice a day.
Clinical variables of women ageing without HIV: The results demonstrated that out of 100 women, 61 women’s height ranged between 151-160 cm, 80 of them weighed between 51-70 kg, 45 had BMI between 19-25, and 40 had blood pressure between 100 mmHg, 60 of them had random capillary blood sugar level between 90- 140 mg/dL; 44 had diabetes, 28 were diagnosed between the ages of 40-45 years and 46-50 years, 42 of them had the illness for less than 5 years, 45 were taking medication for less than 5 years, and 68 of them were taking medication twice a day.
Table 1 shows that all (100%) women aging with HIV had good compliance with the therapeutic regimen. Whereas, among women aging without HIV, majority (92%) had good compliance, 8 percent had fair compliance and none of them had a poor level of compliance with the therapeutic regimen.
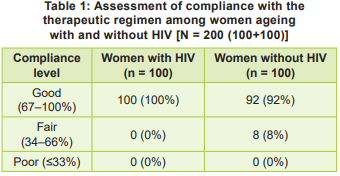
Table 2 shows that the majority (92%) of women ageing with HIV had a good level, and 8 percent had a fair level of HRQoL, whereas, among women aging without HIV, 71 percent had a good level and 29 percent had a fair level of HRQoL, and none had a poor level of HRQoL.
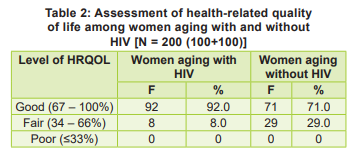
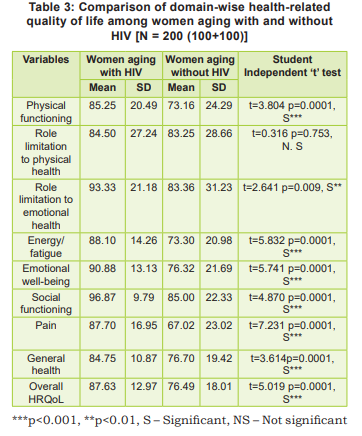
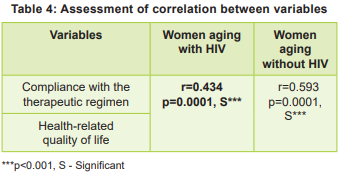
Table 3 shows that there was a statistically significant difference in all domains of HQRoL at 1% level of significance, except in role limitation to physical health. About overall HRQoL the mean score of women aging with HIV was 87.63 with a standard deviation of 12.97. In contrast, the mean score of women aging without HIV was 76.49 with a standard deviation of 18.01, and this difference was statistically significant at 1% level of significance. There was a moderate positive correlation between compliance with the therapeutic regimen and HTQoL among women ageing with and without HIV at 1 percent level of significance (Table 4).
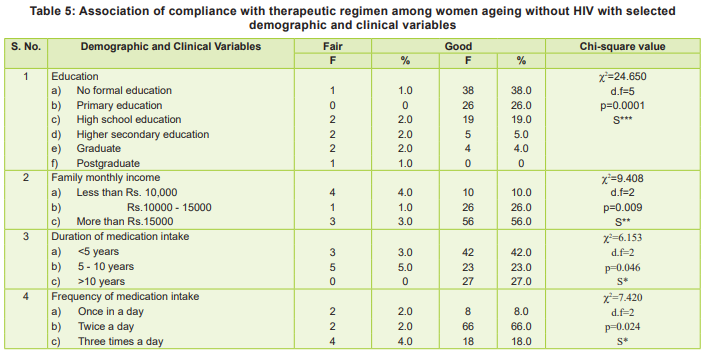
There was a statistically significant association found between compliance with therapeutic regimen among women ageing without HIV and demographic variables such as education and family monthly income, and clinical variables such as presence of medical illness, duration of medication intake, and frequency of medication intake at 5 percent level of significance (Table 5).
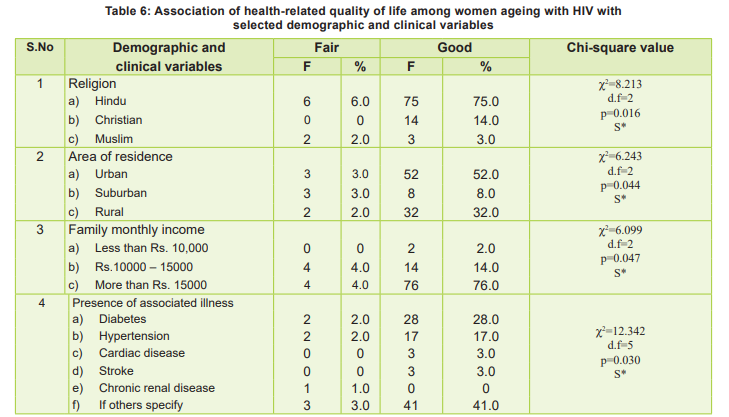
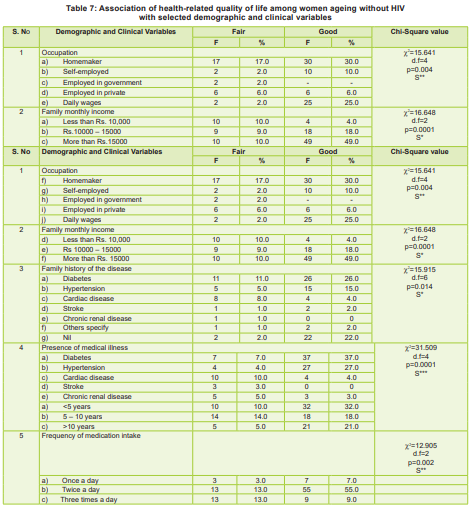
A statistically significant association found between HRQoL among women ageing with HIV and demographic variables such as religion, area of residence, and family income and clinical variables such as Presence of associated illness at 5 percent level of significance (Table 6). Table 7 shows that there was a statistically significant difference between health-related quality of life among women ageing without HIV and demographic variables such as occupation, family income, family history of disease and clinical variables such as presence of medical illness, frequency of medication intake at 5 percent level of significance.
Discussion
All (100%) of women ageing with HIV demonstrated a good level of compliance with the therapeutic regimen. Among women ageing without HIV, the majority (92%) had a good level, while 8 percent had a fair level of compliance. These findings align with a study by Carla (2019), which reported that 95 percent of HIV patients exhibited good or adequate treatment compliance. Similarly, Patel et al (2019) found that 88 percent of hypertensive patients and 82 percent of diabetic patients demonstrating good compliance with prescribed medications.
In terms of HRQoL, the majority (92%) of women ageing with HIV reported a good level, while 8 percent had a fair level. Among women ageing without HIV, 71 percent reported a good level of HRQoL, while 29 percent had a fair level. A statistically significant difference was observed in HRQoL scores between the two groups (p < 0.01), across all domains and the overall score, except for role limitations due to physical health. These findings concur with those of Seguiti & Salvo (2022), who found that HIV-positive patients often had better health-related QoL compared to those with other chronic conditions.
There was a positive correlation between compliance with the therapeutic regimen and the health-related quality of life among women ageing with HIV at 1 percent level of significance. The findings were supported by the study conducted by Johnson et al (2018), which concluded that higher adherence levels contribute to a better quality of life for people living with HIV. The above findings were supported by the systematic review conducted by Shilliday et al (2019), who concluded that better medication adherence is associated with higher health-related quality of life in patients with NCDs.
No statistically significant association was found between compliance with the therapeutic regimen and demographic or clinical variables among women ageing with HIV. The above findings were supported by Okeke et al (2020) who found that there was no association between adherence and clinical factors of patients with HIV, such as CD4 count and viral load.
In contrast, among women ageing without HIV, compliance was significantly associated with the demographic variables of education and family monthly income (p < 0.05), as well as clinical variables such as presence of medical illness, duration of medication intake, and frequency of medication intake (p < 0.05). These findings were similar to those of Garcia et al (2021), which concluded that higher family income was associated with better adherence to the therapeutic regimen. It was also supported in the study by Ingersoll et al (2020), which revealed that duration and frequency of medication intake, along with the presence of other medical conditions, affect adherence to chronic treatment regimens.
Regarding HRQoL among women ageing with HIV, significant associations were observed with demographic variables like religion, area of residence, and family income (p < 0.05). These findings align with Feng & Yang (2021), who reported that family income significantly influenced HRQoL in patients with HIV.
There was also a significant association between HRQoL and clinical variables such as the presence of associated illnesses (p < 0.05) among women with HIV. The findings were consistent with the study results of Bing, et al (2020), which highlighted that the severity of the disease impacts the HRQoL of patients with HIV.
For women ageing without HIV, significant associations were found between HRQoL and demographic variables such as occupation, family monthly income, and family history of disease (p < 0.05), as well as clinical variables including presence of medical illness and frequency of medication intake. The above findings were supported by the study results of Simon (2019), who found that family income affects the HRQoL among individuals with chronic illness and Choi & Yang (2020), who observed that the presence of NCDs negatively impacts quality of life.
Implications for Nursing
Nurse educators can integrate comprehensive modules on the nursing management of patients with HIV and NCDs, emphasising the importance of compliance with therapeutic regimens and their impact on HRQoL. Nurse administrators can develop assessment tools that ensure consistent monitoring of compliance with therapeutic regimen and health-related quality of life of women ageing with and without HIV, and nurse researchers can explore various innovative methods to improve compliance with therapeutic regimen and HRQoL of women ageing with and without HIV
Recommendations
A similar study can be conducted between rural and urban women. In-depth interviews and focus group discussions can be conducted to gain insights into personal experiences and barriers related to compliance with therapeutic regimen among women aging with chronic health issues; a study can be done to assess the effectiveness of nurse-led health promotion packages including mobile health applications and telehealth services, in supporting adherence to therapeutic regimens and monitoring health-related quality of life.
Conclusion
The study results revealed that women ageing with and without HIV had a good level of compliance with the therapeutic regimen and reported good health-related quality of life. Women ageing with HIV showed higher rates of compliance and better health-related quality of life compared to those without HIV. Compliance with the therapeutic regimen was positively correlated with healthrelated quality of life among women ageing with and without HIV. The study also highlighted the influence of demographic and clinical variables on compliance with the therapeutic regimen among women ageing without HIV, and its influence on the health-related quality of life of women ageing with and without HIV. These findings underscore the importance of tailored interventions that consider the unique demographic and clinical profiles of women ageing with and without HIV to improve both compliance and health-related quality of life. The significant correlation between compliance with the therapeutic regimen and health-related quality of life highlights the need for ongoing support to ensure compliance with therapeutic regimens, which, in turn, enhances the overall quality of women.
1. Bing EG, Burnam MA, Longshore D, Fleishman JA, Sherbourne CD, London AS, Shapiro M. The impact of psychiatric conditions on health-related quality of life among people with HIV. American Journal of Psychiatry 2020; 158(2): 178–84 https://doi.org/10.1176/ appi.ajp.158.2.178
2. Carla H. Adherence to antiretroviral therapy among people living with HIV: A cross-sectional study. Journal of Infectious Diseases and Therapy 2019; 7(3): 1-5
3. Choi Y, Yang J. Influence of non-communicable diseases on quality of life among the elderly: A community-based study. Health and Quality of Life Outcomes 2020; 18(1): 212. https://doi.org/10.1186/ s12955-020-01428-7
4. Feng Y, Yang L. Socioeconomic factors associated with quality of life in HIV-positive individuals. BMC Public Health 2021; 21: 347. https://doi.org/10.1186/s12889-021-10397-6
5. Garcia M, Torres R, López J. Socioeconomic determinants of medication adherence in chronic disease management. Journal of Health Economics and Outcomes Research 2021; 9(2): 165-72. https://doi.org/10.36469/jheor.2021.23374
6. ICMR - Indian Council of Medical Research. Health of Women in India: Insights and Challenges, 2018
7. Ingersoll KS, Cohen J. The impact of medication regimen characteristics on adherence in chronic disease management. Journal of Behavioural Medicine 2020; 43(1): 45-46. https://doi.org/10.1007/ s10865-019-00061-y
8. Joshi NK, Sharma P, Patel S, Kumar V. Health-related quality of life related to non-communicable diseases: A descriptive cross-sectional study in Jodhpur, India. Indian Journal of Public Health Research & Development 2021; 12(3): 203-10. https://doi. org/10.1234/ijphrd.2021.012
9. Okeke H, Nwosu B, Onoh R. Factors influencing antiretroviral therapy adherence among HIV patients in sub-Saharan Africa. African Journal of AIDS Research 2020; 19(3): 265-74. https://doi.org/10.2 989/16085906.2020.1786125
10. Patel M, Sharma N, Kumar A. Medication adherence in hypertensive and diabetic patients: A comparative study. International Journal of Medical Science and Public Health 2019; 8(5): 393-97. https://doi.org/10.5455/ijmsph.2019.0208407022019
11. Seguiti F, Salvo L. Quality of life among patients with HIV compared to those with other chronic diseases: A comparative study. Journal of HIV & AIDS 2022; 8(1): 23-29. https://doi.org/10.4172/2327- 5146.1000262
12. Simon A. Influence of socioeconomic status on the health-related quality of life of chronic illness patients. Journal of Chronic Disease Management 2019; 6(2): 101-109
13. Souza HC, Silva RM, Santos MA, Oliveira JP. Adherence to antiretroviral therapy among HIV/AIDS patients: A study of 99 cases. Journal of HIV/AIDS Research 2020; 15(2): 112-23 https://doi. org/10.1234/jhar.2020.015 14. World Health Organisation. India: Country profiles. WHO, 2020

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.